KEYWORDS
LCMUFA
Cetoleic
Gondoic
long- chain monounsaturated fatty acids
olive oil
Skin
Metabolic
Joint
Immunity
Abstract
Fish oils are composed of between 50-100 different lipids. Whilst long chain omega-3 polyunsaturated fatty acids have had extensive research into their health benefits, newer data from preclinical studies are also pointing to health benefits from long-chain monounsaturated fatty acids.
The health benefits shown appear to be complementary to those of omega-3 EPA and DHA. Whilst there is more research needed to understand the underlying mechanisms, one explanation may lie in the differential tissue distribution in the body. Uptake of LCMUFAs in adipose tissue is a candidate for the differential effects seen particularly in metabolic health.
Introduction
Interest in polyunsaturated omega-3 fatty acids was initiated by the groundbreaking work by Danish researchers in the 1970s (1) which showed unexpectedly good cardiovascular health in Innuits despite high dietary intake of fat. Since then, there have been over 40,000 publications showing diverse health benefits of omega-3 fatty acids from prevention of premature births to cardiovascular health, brain health and healthy aging. However, fish oils also contain other, less well researched lipids and recently there has been a series of pre-clinical studies showing that long chain monounsaturates may also be associated with health benefits.
Omega 3-9-11 is a unique combination of bioactive lipids with proposed comprehensive health benefits. With its mix of long chain polyunsaturated (LCPUFAS) and long chain mono-unsaturated fatty acids (LCMUFAs), we believe this oil presents a new opportunity to combine the best of both worlds.
Here we look at the research supporting these fatty acids and where the research is pointing for their best possible use.
Mechanism of action for long chain poly- and mono-unsaturated fatty acids
Those of us working in the omega-3 world are used to hearing that one of the central mechanisms driving omega-3 health benefits is through their anti-inflammatory effects. For omega-3 this is a well-studied concept with evidence from mechanistic studies as well as intervention studies in conditions characterised by chronic inflammation such as rheumatoid arthritis (2), IBD (3) and cardiovascular health (4).
There are several means by which omega-3 can work to reduce inflammation 1) EPA replaces arachidonic acid (AA) on the phospholipid membrane and competes with the COX and LOX enzymes that metabolise AA to prostaglandins, leukotrienes and thromboxane. The metabolism of EPA by COX and LOX enzymes leads to production of less inflammatory eicosanoids. This competitive activity is therefore dependent on the ratio of omega-3 to omega-6, a well described lipid balance that modifies inflammation; 2) EPA and DHA are precursors to specialised pro-resolving mediators (SPMs) which are a highly potent family of molecules that actively dampen inflammation; and 3) omega-3 lipids have a direct effect on immune cells through signalling molecules (e.g. via G-coupled protein receptor 120 on macrophages) (5).
Omega-3, particularly EPA, competes with arachidonic acid, since they are both located on the sn-2 phospholipid and compete for the same metabolic enzymes. Studies determining interactions between LCMUFA and LCPUFA have not been performed and a role of LCMUFA in eicosanoid synthesis or interaction with this pathway is unknown. Most pre-clinical studies with LCMUFA use pollock or saury oil which contain a mix of LCMUFA and LCPUFA. These studies report metabolic benefits of these mixed oils suggesting that there is no clinically significant interference between the two lipid families. Indeed, Yang concludes that the metabolic improvements shown in her study with a mixed oil is due to the combined effects of LCPUFA and LCMUFA (6). Co-incubation studies with lipids in HepG2 cell cultures demonstrated reduced accumulation of fat in cells when LCMUFA and LCPUFA were administered together (7) suggesting the lipid types do not limit each others activities.
Omega-9 and omega-11 LCMUFAs are bioactive lipids present at naturally high levels in some North Atlantic fish species. Documentation of health benefits is less than for omega-3 but they are emerging as lipids with complementary activity to EPA and DHA. Again, the central mechanism behind these benefits is inhibition of chronic inflammation.
The mechanistic data for LCMUFAs is less comprehensive than for the well-studied omega-3s. Yang provided in vivo data (8, 9) showing that LCMUFAs, but not medium chain MUFAs, increase the mRNA expression of PPARg (peroxisome proliferator activated receptor) and possibly PPARa. PPARg promotes fat metabolism and inhibits processes that make fat (de novo lipogenesis). PPAR also affects the expression of important cytokines reducing inflammation. Examples were provided by Yang who showed that LCMUFA supplementation in preclinical studies led to increased adiponectin receptor levels (anti-inflammatory) (8), decreased inflammatory mediators such as CRP (8) and up-regulation of lipid metabolising enzymes in adipocytes (9). Finally, the researchers measured reduced fat content in adipocytes but interestingly no change in triglyceride levels in the liver providing 2 interesting points 1) that LCMUFA activates important lipid metabolising and inflammatory inhibiting pathways, 2) that these biochemical findings translate to actual reduction in risk factors such as lipid content in adipocytes. This rather complex description can be boiled down to the message that LCMUFA reduces inflammation using PPAR signalling; one of main pathways also available to omega-3.
The PPAR receptor is a member of the family of nuclear receptors. These are located in the cytoplasm or nucleus, and upon ligand activation bind directly to DNA, normally as a dimer to promote or inhibit transcription of target genes. PPAR exists in 3 forms a, b/d, and g. Fatty acids tend to bind all 3 regardless of whether they are mono-unsaturated, polyunsaturated, C20 or C22. The receptors are promiscuous in their choice of ligand. PPARs detect the dietary status of the body; if there is too much fat, PPAR is activated to increase fat burning, reduce appetite and lower glucose levels. PPAR is therefore an attractive drug target, and modulation of PPAR activity is how fibrates and glitozone drugs affect metabolic risk factors. Studies using synthetic LCMUFAs show that both gondoic acid and cetoleic acid increase PPAR transcriptional activity to a similar level (10). Since both LCMUFAs and LCPUFAs can act as ligands to PPAR there could be an interaction or competition when giving these fatty acids at the same time however, such interaction studies have not been conducted.
This detailed description is given to demonstrate that PPAR is a common target for LCMUFAs as well as LCPUFAs (omega-3s) and this may account for many lipid-based products claiming to be anti-inflammatory. In other words, at a superficial level there appears to be redundancy – i.e., any fatty acid will work!
This begs the question of why bother taking both LCPUFA and LCMUFA if they do the same thing?
The answer may lie in the differential biodistribution of LCMUFA. Preclinical work by NIH researchers shows striking uptake differences between the LCPUFAs and LCMUFAs in different tissues.
Feeding studies in mice show that LCMUFA is preferentially taken up by adipose tissue whereas n-3 PUFAs show uptake in several tissues with the exception of adipose tissue.
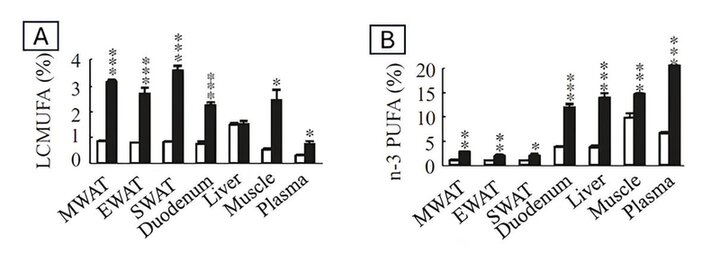
Figure 1 shows the % of LCMUFA or n-3 PUFA from total lipid from various organs from diet-induced obese C57BL/6 J mice. Panel A shows the LCMUFA content in tissues following supplementation for 18 weeks with saury oil (high in LCMUFA). Panel B shows the omega-3 PUFA content in tissues following supplementation for 18 weeks with saury oil. MWAT= mesenteric white adipose tissue, EWAT = epididymal white adipose tissue, SWAT = sub-cutaneous white adipose tissue.
White adipose tissue stores excess fat in the form of triglycerides and plays a key function in sensing and controlling fluctuations in dietary energy intake. A consequence of this is that adipocytes are central in dietary metabolic regulation, particularly insulin sensitivity and glucose metabolism as well as cholesterol regulation. Adipocytes communicate with themselves (autocrine), adjacent cells (paracrine) and throughout the body (endocrine) by release of hormones termed adipokines. Adipokines can be pro-inflammatory or anti-inflammatory. Adiponectin is an example of the latter and has a key role in metabolic health. This hormone increases insulin sensitivity in muscle and liver, reduces plasma glucose and increases use of fat as energy (11). Adiponectin also has an important anti-inflammatory role and there is increasing evidence that chronic mild inflammation is associated with insulin resistance. Pre-clinical evidence suggests that adiponectin increases insulin sensitivity signalling in liver and muscle by reducing adipocyte related inflammation (12). Interestingly, adiponectin levels are highly associated with obesity such that increasing obesity leads to lower levels of adiponectin. This may be crucial since obesity is also associated with chronic low-grade inflammation.
We therefore propose that LCMUFAs have activity via adipocyte mediated effects, whereas omega-3 lipids have a more systemic impact (with the exception of adipose tissue). This hypothesis is likely to be a simplification, and there is likely to be a degree of overlap in the biodistribution and function of specific lipids, but as a basic principle it may provide an explanation for the documented differential effects of LCMUFAs and LCPUFAs.
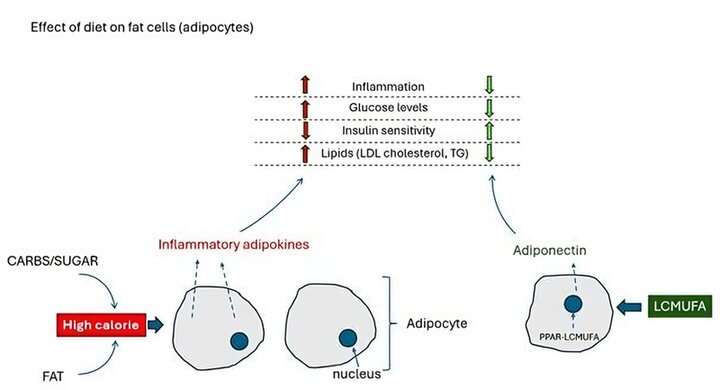
Figure 2: Effect of LCMUFA on fat cells (adipocytes)
The effects of LCMUFA appear to be complementary to those of EPA and DHA with regards to metabolic health. On one hand EPA/DHA have beneficial effects on triglycerides, HDL levels (good cholesterol), blood pressure and liver fat accumulation (hepatic steatosis), whereas LCMUFAs regulate insulin sensitivity and non-HDL cholesterol (6). This has been documented in a series of preclinical studies demonstrating the effects of LCMUFA on total- and LDL-cholesterol (13, 14), glucose and insulin levels (9, 14) as well as a potential combined effect when provided with omega-3 (7). Combining the fatty acids may therefore provide comprehensive metabolic protection.
Skin biology
Sub-cutaneous fat is the largest fat storage compartment in the body and this may have a significant impact on skin health (15). Observational studies suggest there is a relationship between obesity, inflammation and atopic dermatitis, there is also a reduction in adipokine levels with obesity (particularly adiponectin), and a strong association between lowered adipokine levels and atopic dermatitis (16-18).
This has led to the proposal that adipose tissue inflammation is implicated in the pathogenesis of atopic dermatitis and psoriasis (15).
These findings, together with the evidence that LCMUFAs show substantial uptake in sub-cutaneous fat and act as anti-inflammatory agents, supports the hypothesis that LCMUFAs may support skin health, with adiponectin or other adipokines playing a key role in skin regulation.
Epax has performed a pilot study showing that an LCMUFA rich oil significantly reduced the redness in facial skin measured using a VISIA machine compared to placebo (19). The study was well controlled to prevent redness from temperature changes, exertion and use of make-up or creams and for seasonal effects on skin.
The finding from the pilot study provide an indication that LCMUFA rich oils may reduce skin inflammation and help maintain skin function. These findings give encouragement for the design of a new skin health study with the working hypothesis that LCMUFA reduces adipocyte derived inflammatory mediators important in skin health. The study protocol includes lipidomic measurements of the skin to also determine additional effects on lipid composition of the epidermis.
Omega-3 is known to reduce skin sensitivity shown by studies performed using UVB as a means of controlled insult to the skin. In these studies the minimal erythemal dose (dose needed to get sunburn) increased in subjects taking omega-3 supplementation (20). UVB penetrates the skin but is unlikely to reach sub-cutaneous fat (UVA penetrates even less). The effect of omega-3 in UV protection is therefore most likely on the epidermis and dermis (on keratinocytes, melanocytes and immune cells). Omega-3 also improves skin water retention, promotes skin health after damage and reduces inflammatory conditions and protects from photoaging (21, 22, 23).
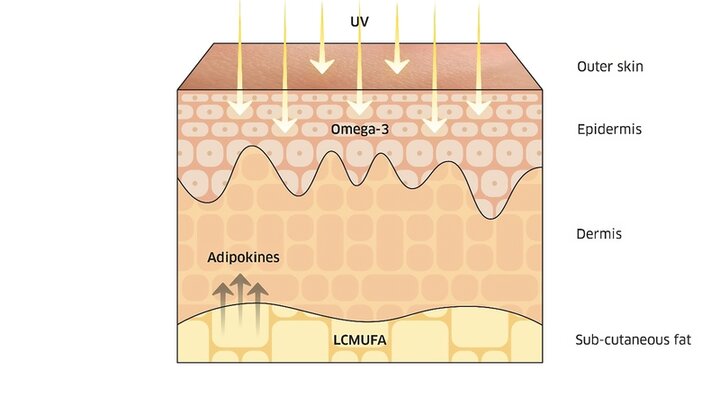
Figure 3. Skin structure and how the biodistribution of omega-3 and LCMUFA may act together to give comprehensive skin protection.
Differential localisation of LCMUFA to subcutaneous fat and omega-3 to the dermis and epidermis may therefore provide another example of a mixed oil providing a comprehensive health benefit. However, it should also be noted that the differential uptake of LCMUFA and omega-3 in skin has not yet been demonstrated in humans.
We therefore propose the hypothesis that a combination of LCPUFA-omega-3 with LCMUFAs can provide a comprehensive health effect particularly where adipose tissue is an important contributing factor.
Conflict of interest declaration
Derek Tobin is an employee of Epax Norway AS.
Conclusion
Looking ahead, the aging population will have a huge impact on the future healthcare landscape.
With nearly 12.0% of the world's population aged 65 and over by 2030, age-related health issues such as memory loss, incontinence, mobility problems and eye/vision problems will continue to rise and become a major concern for consumers.
Lifestyle-related diseases and mental health issues will continue to be major health concerns, particularly in developing countries where rapid urbanization and changing work/life conditions are having a major impact on people's diets, physical activity and social relationships.
Driven by technology and innovation, consumers around the world are becoming increasingly informed about health issues and their health status. Understanding their health behaviors and anticipating their future needs is critical for companies today.
With the rise of stress and anxiety, mental and emotional health will continue to grow in importance as consumers seek happiness as the ultimate form of health status.
The commercialization of "happiness" may be a future prospect, as a large proportion of global consumers already associate health with mental wellbeing.
References and notes
1. Bang HO, Dyerberg J, Nielsen AB. Plasma lipid and lipoprotein pattern in Greenlandic West-coast Eskimos. Lancet. 1971;1(7710):1143-5.
2. Miles EA, Calder PC. Influence of marine n-3 polyunsaturated fatty acids on immune function and a systematic review of their effects on clinical outcomes in rheumatoid arthritis. Br J Nutr. 2012;107 Suppl 2:S171-84.
3. Calder PC. Fatty acids and immune function: relevance to inflammatory bowel diseases. Int Rev Immunol. 2009;28(6):506-34.
4. Watanabe Y, Tatsuno I. Prevention of Cardiovascular Events with Omega-3 Polyunsaturated Fatty Acids and the Mechanism Involved. J Atheroscler Thromb. 2020;27(3):183-98.
5. Oh DY, Talukdar S, Bae EJ, Imamura T, Morinaga H, Fan W, et al. GPR120 is an omega-3 fatty acid receptor mediating potent anti-inflammatory and insulin-sensitizing effects. Cell. 2010;142(5):687-98.
6. Yang ZH, Inoue S, Taniguchi Y, Miyahara H, Iwasaki Y, Takeo J, et al. Long-term dietary supplementation with saury oil attenuates metabolic abnormalities in mice fed a high-fat diet: combined beneficial effect of omega-3 fatty acids and long-chain monounsaturated fatty acids. Lipids Health Dis. 2015;14:155.
7. Yoshinaga K, Mizuno Y, Senarath S, Yoshinaga-Kiriake A, Nagai T, Beppu F, et al. Simultaneous Treatment of Long-chain Monounsaturated Fatty Acid and n-3 Polyunsaturated Fatty Acid Decreases Lipid and Cholesterol Levels in HepG2 Cell. J Oleo Sci. 2021;70(5):731-6.
8. Yang ZH, Bando M, Sakurai T, Chen Y, Emma-Okon B, Wilhite B, et al. Long-chain monounsaturated fatty acid-rich fish oil attenuates the development of atherosclerosis in mouse models. Mol Nutr Food Res. 2016;60(10):2208-18.
9. Yang ZH, Miyahara H, Iwasaki Y, Takeo J, Katayama M. Dietary supplementation with long-chain monounsaturated fatty acids attenuates obesity-related metabolic dysfunction and increases expression of PPAR gamma in adipose tissue in type 2 diabetic KK-Ay mice. Nutr Metab (Lond). 2013;10(1):16.
10. Yang ZH, Gordon SM, Sviridov D, Wang S, Danner RL, Pryor M, et al. Dietary supplementation with long-chain monounsaturated fatty acid isomers decreases atherosclerosis and alters lipoprotein proteomes in LDLr(-/-) mice. Atherosclerosis. 2017;262:31-8.
11. Greenberg AS, Obin MS. Obesity and the role of adipose tissue in inflammation and metabolism. Am J Clin Nutr. 2006;83(2):461s-5s.
12. Kawai T, Autieri MV, Scalia R. Adipose tissue inflammation and metabolic dysfunction in obesity. Am J Physiol Cell Physiol. 2021;320(3):C375-c91.
13. Yang ZH, Miyahara H, Takeo J, Hatanaka A, Katayama M. Pollock oil supplementation modulates hyperlipidemia and ameliorates hepatic steatosis in mice fed a high-fat diet. Lipids Health Dis. 2011;10:189.
14. Yang ZH, Miyahara H, Mori T, Doisaki N, Hatanaka A. Beneficial effects of dietary fish-oil-derived monounsaturated fatty acids on metabolic syndrome risk factors and insulin resistance in mice. J Agric Food Chem. 2011;59(13):7482-9.
15. Guo Z, Yang Y, Liao Y, Shi Y, Zhang LJ. Emerging Roles of Adipose Tissue in the Pathogenesis of Psoriasis and Atopic Dermatitis in Obesity. JID Innov. 2022;2(1):100064.
16. Jung MJ, Kim HR, Kang SY, Kim HO, Chung BY, Park CW. Effect of Weight Reduction on Treatment Outcomes for Patients with Atopic Dermatitis. Ann Dermatol. 2020;32(4):319-26.
17. Jaworek AK, Szepietowski JC, Szafraniec K, Jaworek M, Hałubiec P, Wojas-Pelc A, et al. Adipokines as Biomarkers of Atopic Dermatitis in Adults. J Clin Med. 2020;9(9).
18. Lee SH, Bae Y, Park YL. Clinical Implication of Serum Adiponectin Levels in Adult Patients with Atopic Dermatitis. J Clin Med. 2022;11(21).
19. Tobin D, Midtbø LK, Mildenberger J, Svensen H, Stoknes I. The effect of fish oil rich in cetoleic acid on the omega-3 index and skin quality. Prostaglandins Leukot Essent Fatty Acids. 2024;201:102616.
20. Rhodes LE, O'Farrell S, Jackson MJ, Friedmann PS. Dietary fish-oil supplementation in humans reduces UVB-erythemal sensitivity but increases epidermal lipid peroxidation. J Invest Dermatol. 1994;103(2):151-4.
21. Huang TH, Wang PW, Yang SC, Chou WL, Fang JY. Cosmetic and Therapeutic Applications of Fish Oil's Fatty Acids on the Skin. Mar Drugs. 2018;16(8).
22. Koch C, Dölle S, Metzger M, Rasche C, Jungclas H, Rühl R, et al. Docosahexaenoic acid (DHA) supplementation in atopic eczema: a randomized, double-blind, controlled trial. Br J Dermatol. 2008;158(4):786-92.
23. Tveit KS, Brokstad KA, Berge RK, Sæbø PC, Hallaråker H, Brekke S, et al. A Randomized, Double-blind, Placebo-controlled Clinical Study to Investigate the efficacy of Herring Roe Oil for treatment of Psoriasis. Acta Derm Venereol. 2020;100(10):adv00154.



